

Wisdom teeth are a pain. Most of us don’t have room for them and end up having them removed. The long and the short of it is, “If you have impacted wisdom teeth, unless they are deeply buried under the bone, you should have them removed, and the sooner you do this, the better.”
We can help you determine whether or not you should be worried about your wisdom teeth, what treatment might be required in your individual circumstances, and what the costs might be.
Chances are, we will be able to carry out any necessary procedure in our pleasant, comfortable offices at a time that suits you. With the benefits of a little sedation and some local anaesthetic, you will find the experience a lot less dramatic than your friends would have you believe.
If you really want to know more, you should find the answers to your questions below. Better still, call us for an appointment to discuss.
Q. What are wisdom teeth?
A. Wisdom teeth (also known as third molars) are teeth that appear at the very back of the mouth usually between the ages of 18 and 25 years. They are the last of the adult permanent teeth to develop.
Q. Are all wisdom teeth problematic?
A. No. If wisdom teeth come fully through, they can be useful teeth. If they are kept healthy by careful cleaning, they will last a lifetime.
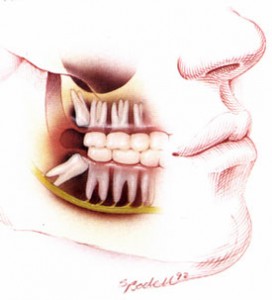 Q. What are ‘impacted’ wisdom teeth?
Q. What are ‘impacted’ wisdom teeth?
A. Because they are the last teeth to develop, there is usually not enough room for wisdom teeth, so they only come through part-way or not at all. These cases are called ‘impacted’ wisdom teeth.
Q. Why are impacted wisdom teeth a problem?
A. There are a number of reasons:
Q. Do I need to have my impacted wisdom teeth removed?
A. It depends. If you are 25 years old or younger and have impacted wisdom teeth, you are almost certainly better off having them removed. If you are over thirty, the situation is a little more complicated. For ‘over-thirtys’, if the wisdom teeth are completely covered with bone on an X-ray, they can probably be left (such teeth should be periodically reviewed by your dentist). If the wisdom teeth are partially through into the mouth, however, they should probably removed in most cases. As with any surgical procedure, a risk analysis should be undertaken by an experienced dental or oral surgeon, to determine the risks profile of surgery as opposed to the risk profile of leaving the teeth in place. This will require a clinical examination, history taking and a special X-ray.
Q. Why should I have my impacted wisdom teeth removed if they have not given any trouble?
A. As mentioned above, unless impacted wisdom teeth are well covered by bone they are almost certain to cause problems if left in place. This is particularly true of the lower wisdom teeth. Such problems can occur suddenly, and often at the most inconvenient times.
Q. When should I have my impacted wisdom teeth removed?
A. Immediately after any acute infection has been controlled. It is now recommended by most specialists that impacted wisdom teeth should be removed between the ages of 14 and 25 years, whether they are causing problems or not. Surgery is technically easier and patients recover much more quickly when they are younger. What is a relatively minor operation at 20 years of age can become quite difficult in patients over 40. Also, the risk of complications increases with age, and the healing process is slower.
As a rule, removal of wisdom teeth is regarded as an elective procedure, but should be carried out at the earliest convenient time. Don’t wait until you have pain, swelling or infection.
Athletes who have impacted wisdom teeth should have their surgery carried out in the ‘off-season’, if possible.
Q. How are wisdom teeth removed?
A. There are three options here:
Q. If my wisdom teeth need to be removed, who will do it?
A. Straightforward removal of wisdom teeth may be done by your regular dentist. More complex extractions will often require referral by your dentist for treatment. We receive referrals from a large number of dentists for wisdom tooth surgery on a regular basis. Dr Neil Piccione is experienced at the surgical management of impacted wisdom teeth, and he is certified to administer intravenous sedation. It is very likely that he will be able to help you.
If your are assessed as requiring a general anaesthetic, we can assist you to find a surgeon and facility that will be able to help you.
Q. How does it all work?

A. Make an appointment for a consultation with your dentist or call our office. If your dentist is not prepared to undertake the treatment themselves, they will refer you to someone else.
If you are referred to us (or come to us on your own), our office procedure is as follows:
You will need to have a special X-ray done (often called an OPG or Panex) and this should be available to us at your consultation appointment (we can arrange this for you).
We will then need a consultation appointment to meet you and discuss treatment with you before scheduling an appointment for surgery. At this initial consultation appointment, your specific treatment needs will be assessed and discussed. Your general health and medical history will be reviewed. Any risk factors will be identified, explained and discussed. The procedure will be explained to you and you will have an opportunity to ask any questions. An estimate will be prepared and a consent form presented to you for your signature. You will then be able to make an appointment for surgery.
Q. What do I have to do to prepare for surgery?
A. Please take note of the following if you are having surgery under intravenous sedation:
You should not have anything to eat or drink (‘nil per mouth’) for four hours before surgery (insulin dependent diabetics may require special attention – please discuss with Dr Piccione).
Q. Will it hurt?
A. You will not feel any pain during the procedure.
Q. How much does it cost?
A. This varies depending on the number of teeth involved, the need for special tests or X-rays, the time required and the complexity of the surgery. As a guide, our recent fees for wisdom tooth surgery under intravenous sedation have varied between NZ$800 and NZ$2100. A written estimate will be given to you after your consultation appointment (before you make your surgery appointment). We do require payment in full on the day of surgery.
Q. How long will it take?
A. You should plan on being at the surgery about an hour, sometimes a little longer. Please instruct your escort/driver to arrive 45 minutes after your appointment begins, so that we can go over your care instructions with them and answer any questions they may have.
Q. What can I expect after wisdom tooth surgery?
A. Surgical removal of wisdom teeth does cause more discomfort than routine extractions. After the local anaesthetic wears off, usually several hours after you get home, you may experience:
All these symptoms are temporary , and in most cases your mouth will be feeling normal within a few weeks.
You should be seen a week after surgery to check healing and remove any sutures (stitches). This is usually a short appointment of 5-10 minutes duration.
Q. What is a ‘dry socket’?
A. This is a painful condition that usually begins 3-4 days after tooth extraction. It most commonly occurs after the removal of lower wisdom teeth, and is seen much more often in smokers. It is characterised by an empty tooth socket (no blood clot), and increasing pain. Treatment usually consists of placing a dressing in the wound to disinfect the area and make it more comfortable while healing occurs. Antibiotics are sometimes also prescribed.
Q. Is it normal to still have tingling or a numb feeling in my lip, chin or tongue several days after having wisdom teeth out?
A. No, but this is a well-known complication of wisdom tooth surgery that is explained during the initial consultation and consent procedure. It is generally due to injury to one of the nerves that lies close to the wisdom tooth that was removed. The tingling/numbness usually returns to normal with time, although it may be permanent. This complication is said to occur in up to 10% of people, but is much less common in younger patients (under the age of 20 years). You should contact us if you experience this complication.
Q. Will the antibiotics prescribed make my oral contraceptive less effective?
A. Yes, this is a distinct possibility. While you are taking the antibiotics and for the next seven ‘real’ pill days, you should use additional contraceptive measures.
Q. What should I do after surgery?
A. You will be given specific written instructions. In general:
Q. What about post-operative care of my mouth?
A. You will be given specific written instructions. In general:
 Do not smoke for 36 hours. Smoking will promote bleeding and interfere with healing.
Do not smoke for 36 hours. Smoking will promote bleeding and interfere with healing.Q. How long before I can go back to work?
A. Different people recover from wisdom tooth surgery at different rates. Depending on the nature of the surgery, your age and your individual recovery capacity, you should expect to get back to regular work in 2-4 days. In our practice, most people choose to have their surgery on a Thursday or Friday and almost all are fine to return to work by the following Monday.
Please Note: If you are uncertain whether or not to proceed with any suggested treatment, it is a good idea to get a second opinion. The decision to proceed with treatment (or not) is yours, and should be made only after you are fully informed.
