

Endodontics is the field of dentistry that deals with treating the diseased pulp (or “nerve”) inside a tooth.
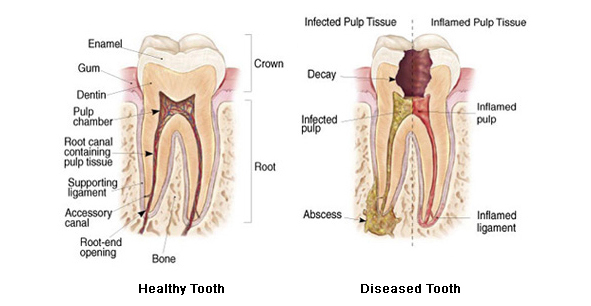
Advanced decay or a physical injury can damage the pulp inside the tooth. The pulp can become infected. Tooth pulps sometimes degenerate and die due to chronic trauma (such as in people who clench or grind their teeth). This can also happen under deep fillings or crowns – often years after the original dentistry was done.
Early signs of pulp inflammation are temperature sensitivity, teeth over-react to hot or cold. This can sometimes be reversed with anti-inflammatories in conjunction with removing the irritant, if one can be identified (decay, cracks in teeth or a high filling). Once a pulp space is infected or the pulp has died, it is inevitable that an abscess will form.
Once an abscess forms, the signs and symptoms change. While temperature sensitivity (usually to hot rather than cold) might continue, there is increasing pain and increasing tenderness to bite on the tooth. The affected tooth may feel ‘high’. There may be tenderness or swelling or discharge from the gum adjacent to the affected tooth. Once these features are present, the treatment choices are limited – extraction or root canal treatment.
Deciding which one is appropriate for you will require a physical examination and an X-Ray or two.
X-Rays (Radiographs)
 During a root canal treatment, your dentist will need to take X-ray images of the tooth to determine the position of the instruments and filling material inside the root canals. An electronic “apex locator” may also be used in determining the length of the root canals.
During a root canal treatment, your dentist will need to take X-ray images of the tooth to determine the position of the instruments and filling material inside the root canals. An electronic “apex locator” may also be used in determining the length of the root canals.
Access opening
Treatment is done under local anaesthetic, to ensure your comfort. First the dentist will remove any decayed and weak tooth structure. An opening into the pulp chamber is then prepared to allow access to the root canals of the tooth.
Instrumentation
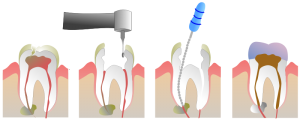 The root canals are accessed, measured and then cleaned out with special root canal files. Some files are used by hand, others rotate in a handpiece. The canals are carefully cleaned, smoothed and shaped. During canal filing, the inside of the tooth is frequently washed out with a special disinfectant solution. In most cases, the canals are then dressed with antiseptic medications and the tooth is sealed with a temporary filling material for a week or two to allow time for the acute infection to settle. Antibiotics are sometimes prescribed.
The root canals are accessed, measured and then cleaned out with special root canal files. Some files are used by hand, others rotate in a handpiece. The canals are carefully cleaned, smoothed and shaped. During canal filing, the inside of the tooth is frequently washed out with a special disinfectant solution. In most cases, the canals are then dressed with antiseptic medications and the tooth is sealed with a temporary filling material for a week or two to allow time for the acute infection to settle. Antibiotics are sometimes prescribed.
Sealing
Once the canals are infection free, they can be sealed. A root filling material (usually a rubbery material called ‘gutta percha’) is placed into each canal, together with a special paste sealer.
Final restoration
 Placing a good final restoration is as important as the root canal treatment itself. If the restoration leaks, bacteria can work their way back down the root canal sealer and re-infect the tooth. A permanent filling is placed into the access opening. Teeth with large amounts of damage may need a post down one or more canals to anchor the filling securely onto the root of the tooth.
Placing a good final restoration is as important as the root canal treatment itself. If the restoration leaks, bacteria can work their way back down the root canal sealer and re-infect the tooth. A permanent filling is placed into the access opening. Teeth with large amounts of damage may need a post down one or more canals to anchor the filling securely onto the root of the tooth.
Root treated teeth are more susceptible to cracking or splitting. Dentists often recommend that root treated teeth are restored with crowns, so that the risk of catastrophic fracture is significantly reduced.
Risks and complications
Despite our best efforts, a small percentage of root treatments fail. The failure rate is higher for re-treatments (where a previous root treatment has failed). It is important to realise that root canal treatment is an alternative to extraction. While most root filled teeth are successfully saved from extraction for many years, extraction may be required in some cases.
Despite the greatest care being taken, occasionally the files used to clean the inside of the tooth separate (break off) in the canals. This usually happens in very fine or very curved roots. Sometimes these are retrievable but they may also be sealed in the root canal as part of the filling.
What happens if I don’t have a root canal treatment?
A dental abscess is no trivial matter. Prior to the days of antibiotics, dental infections were not uncommonly fatal, due to swelling that obstructed the airway. Even now, people with certain medical conditions who have compromised immune systems, damaged or artificial heart valves or artificial joints are at risk of serious complications if bacteria from a dental infection get into the bloodstream.
Are there any alternative treatment options?
Only extraction.
